Defining Vitreoretinal Lymphoma
- Contents:
Diagnosis of VRL
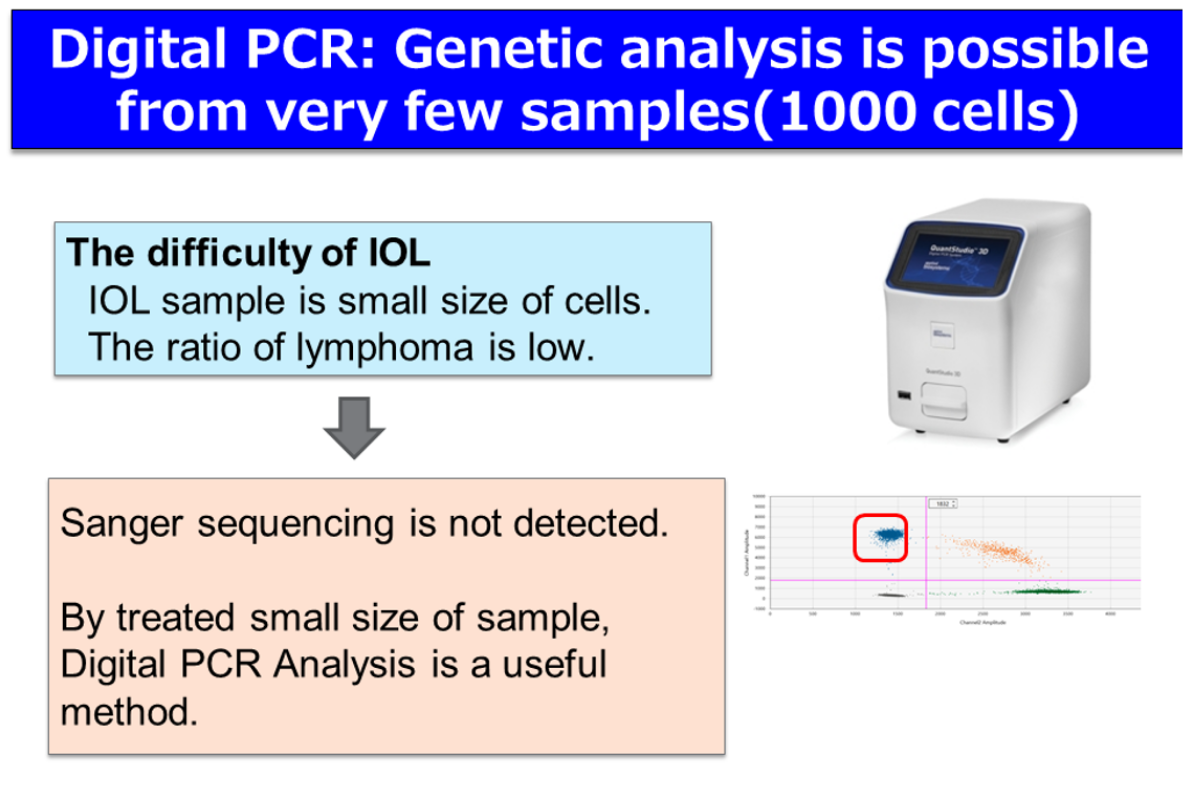
The definitive diagnosis of PVRL relies on the proof of malignant lymphoma cells in the Vitreoretinal fluid. To obtain large quantities of malignant lymphoma cells, the Vitreous opacity should be as high as possible when conducting the Vitreous biopsy. In the case of retinal invasion of lymphoma cells, a retinal biopsy should be conducted. However, this diagnosis may be difficult if cell counts or the concentration of tumor cells is low. In such a case, PVRL diagnosis based on cytology, along with the concentration of IL-10/IL-6 (>1), IgH gene reconstruction, and Flow Cytometric Analysis (FACS), should be practiced. In addition, adjunctive diagnosis using MYD88 L265P mutation and CD79B mutation in the Vitreoretinal fluid have been utilized for lymphoma diagnosis.
In the initial staging, brain MRI, cytological diagnosis, and ideally cerebrospinal fluid examination including flow cytometric analysis, as well as systemic enhanced CT or PET-CT, and bone-marrow biopsy are required.
B-cell receptor (BCR) signaling plays a central role in the survival, activation, proliferation, maturation, and differentiation of B cell lymphoma cells. It is particularly noted that the BCR signaling pathway in non-Hodgkin Lymphoma (B-NHL), known as the Burton Tyrosine Kinase, is permanently activated. Approximately 95% of VRL are B-cell lymphomas with activated Burton Tyrosine Kinase. The administration of BTK inhibitors targeting patients with CNS lymphoma has reported an efficacy of ORR of 77% (Grommes et al, 2017).
BTK inhibitors exhibit a high intracerebral transferability and are one of the effective therapeutic agents against VRL. This study hypothesized that by using Burton Tyrosine Kinase inhibitors, BTK inhibitors could efficiently suppress cerebral relapse. Maintenance therapy with BTK inhibitors after complete remission of VRL may provide improved effectiveness in relation to visibly undetectable microinvasions in the brain.